CROATIAN SCIENCE FOUNDATION – INSTALLATION GRANTS – UIP-09-2014
Biomarkers in schizophrenia – integration of complementary methods in longitudinal follow up of first episode psychosis patients
In Croatian: Biomarkeri u shizofreniji – integracija komplementarnih pristupa u praćenju osoba s prvom psihotičnom epizodom, Number: 110316 HRZZ
PROJECT LEADER
Associate professor Martina Rojnić Kuzman, M.D., Ph.D., psychiatrist, Zagreb School of Medicine and University Hospital Centre Zagreb.
PARTNER INSTITUTIONS
University Hospital Centre Zagreb (Department of psychiatry, Department of neurology, Department of laboratory diagnostics, Department of nuclear medicine), University hospital Vrapče, Psychiatric Hospital Sveti Ivan, Psychiatric hospital Dr.Ivan Barbot (Croatia); and Pharmacogenetics Research Clinic, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto (Canada).
COLLABORATORS
Associate professor Marina Boban, M.D., Ph.D., neurologist; Dina Bošnjak, M.D., psychiatry trainee; Tamara Božina, M.D., Ph.D; professor Nada Božina, M.D., Ph.D.; associate professor Sanja Darmopil, Ph.D.; associate professor Igor Filipčić, M.D., Ph.D., psychiatrist; Lana Ganoci, mr.sc.biotech., Vladimir Grošić, M.D., Ph.D., psychiatrist; Ana Hladnik, M.D.; Ivana Kekin, M.D., psychiatrist; Porin Makarić, M.D., psychiatry trainee; Nina Mayer, M.D., psychiatrist; Zoran Madžarac, M.D., psychiatrist; associate professor Branko Malojčić, M.D., Ph.D., Ratimir Petrović, M.D., Linda Rossini Gajšak, M.D., psychiatry trainee; Aleksandar Savić, M.D., psychiatrist; associate professor Marina Šagud, M.D., Ph.D., Željka Vogrinc, M.D., Ph.D.; Maja Živković, M.D., Ph.D., psychiatrist; associate professor Daniel Mueller, M.D., Ph.D.
STUDY DURATION
2015 - 2018
SUMMARY OF PROJECT
Schizophrenia is one of the most disabling psychiatric illnesses, affecting about 1% of population worldwide. Although the term schizophrenia is used to describe a relatively heterogeneous group of clinical presentations, in majority of cases, schizophrenia is a chronic illness with a recurrent course, characterized by alternating periods of acute psychotic illness and their remission. A prodromal stage which may last for several years prior to presentation of acute psychotic symptoms usually precedes the first acute psychosis. Duration of at least six months of the first episode of psychosis is highly suggestive of schizophrenia. The pathogenesis of this illness is still largely unknown and the diagnosis of schizophrenia is based on its clinical presentation. To objectify the diagnosis and course of treatment of this illness, huge efforts have been made to identify a biological correlate of schizophrenia yet without straightforward results. In the rapidly growing field of genetics and pharmacogenomics using the most sophisticated technology (genome-wide association studies (GWAS)) with a large number of samples, a number of genetic markers have been proposed as associated with the progression of illness and/or treatment response. However, the concordance even among the results of these studies is rather modest. Thus, the methodology in the search for biomarkers has to be revised in order to enhance the power of its findings.
To achieve that goal, a more systematic approach is needed: 1) with the exception of few new studies emerging in the literature, there is a need for longitudinal studies on well defined samples of first episode schizophrenia (FEP) patients to overcome the confounders from previous studies (i.e. cross sectional design, short follow up of patients, heterogeneous sample of patients in the aspects of clinical presentation of symptoms dimensions, patterns of relapse, regain of functioning after an acute episode of illness and cognitive functioning, confounding effects of medication); 2) even with FEP studies, there is a clear need to integrate different approaches when searching for biomarkers. A large body of genetic studies concluded that schizophrenia results from the gene x environment interaction and once again revitalized the stress diathesis model of schizophrenia. This model implies that the interaction of genes and environment shape the vulnerability to schizophrenia. When the final stress hits the vulnerable person, schizophrenia will occur. Indeed, a significant number of findings of patients in schizophrenia, even in FEP could be related theoretically to alterations in stress response/ stress diathesis model and replicate the findings from animal studies, starting from altered hypothalamus – pituitary – adrenal (HPA) axis functions, a clear indicator of stress response, to alterations in immune system, neurocognitive dysfunctions, increased sensitivity to psychosocial stress, reductions in hippocampal volume and activated microglia in the brain. Thus, we plan to examine a set of biomarkers according to the stress diathesis model including the psychopathological status, neurocognitive functioning and stress response by using brain functional and neuroimaging (single photon emission computed tomography – SPECT) methods in 150 FEP patients vs. controls and their changes during the FEP and subsequent remission in 18-month longitudinal follow up. Secondly, we will examine the course of treatment of previously non medicated FEP patients by using pharmacogenetic analysis. GWAS will be performed in collaboration with the research group of Toronto, further expanding our international collaboration. Third, we will study alteration in number and distribution, as well as morphology and chemical properties of specific neuron subclasses in histologically prepared human cortical tissue of post mortem samples of schizophrenic subjects in the region that synaptic alteration was suggested by in-vivo functional and structural imaging (SPECT) and psychological.
This project will be a continuation of our previous studies, including several reports where we showed significant alterations in drug naive FEP subjects. In example, we found significant gene expression changes that occur in the FEP vs. controls, and in subsequent remission in newly-diagnosed patients with schizophrenia that might possibly serve as biomarkers of the disease progression. Likewise, we identified pharmacogenetic markers possibly associated with susceptibility to metabolic side effect to antipsychotic treatment. However, this research project brings an innovative multidisciplinary approach to identify biomarkers based on the stress diathesis model in schizophrenia at clinical, functional, structural and genetic level in vivo as well as on neuronal level in postmortal tissue. The unique contribution of this research include clear clinical implications and scientific implications, since with this project we will gather a substantial amount of relevant clinical data on the subject of FEP during longitudinal follow up. Therefore, we believe that the results of this study will contribute to the scientific knowledge on international level.
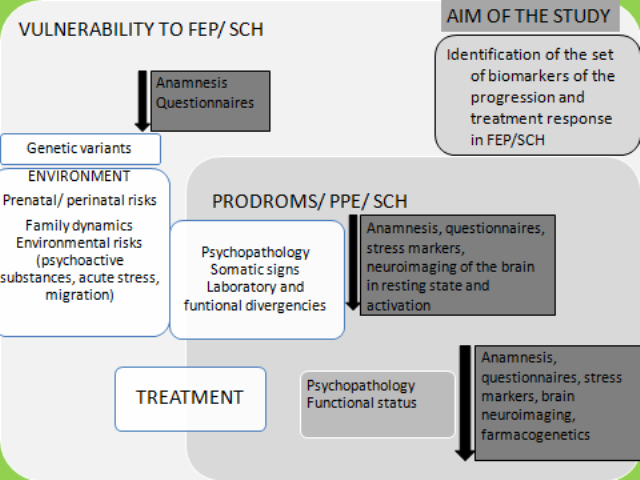
Figure 1. The concept of the study, based on the comprehensive model of the development and treatment of FEP and schizophrenia
STUDY AIMS, METHODS AND EXPECTED RESULTS
General aims:
- to examine a set of biomarkers in FEP patients vs. controls and their changes during the FEP and subsequent remission in patients during longitudinal follow up
- to examine the course of treatment of previously non medicated FEP patients in several aspect of functioning during longitudinal follow up
Specific objectives and expected results are related to four complementary areas of research, performed through different work packages (WP1-WP4):
WP1 – contains all clinical assessment at baseline and during follow up that are necessary for WP2 and WP4. These data do not necessary generate new and unknown results in the field of schizophrenia research, but may confirm the existing data. The aim of WP1 is to examine baseline clinical and laboratory features in FEP patients and their changes during a minimum of 1, 5 year treatment with antipsychotics. In relation to this aim, our hypotheses are: 1. Psychopathology, emotional recognition and neurocognitive status will improve after 1, 5 year of treatment with significant differences in their degree of improvement among patients; 2. Alterations of hormones and lipids will be observed as baseline alterations as well as side effects to treatment; first, we expect to prove these hypotheses. Secondly, we will use these data to perform the association study described under WP2 and WP4.
WP2 – uses as subgroup of patients where additional analyses will be performed aiming to elucidate the mechanisms underlying neurocognitive and emotional deficits at the beginning of the illness as well as during the treatment. Specific aims include:
- to examine baseline alterations of the blood flow velocities (BFV) and pulsatility in the main intracranial arteries and the cerebral blood flow (CBF) changes using transcranial Doppler sonography (TCD) in relation to neurocognitive and stress paradigm in FEP subjects compared to control subjects, at baseline and after 1.5 years of treatment
- to examine baseline alterations of the regional cerebral flow (rCBF) using SPECT and its changes in relation to 1.5 year treatment with antipsychotics in FEP patients and to correlate is with psychopathology, neurocognitive status and emotional recognition status
- to examine the correlation of SPECT rCBF with alterations of the blood flow velocities (BFV) and pulsatility obtained during neurocognitive and stress paradigm
- to examine the analysis of difference in stress response patterns in patients and controls measured with cortisole increase during stress paradigm, and their changes in relation to 1.5 year treatment with antipsychotics in FEP
WP3 incorporates the post mortem analysis, based on the results from WP3. We will study alteration in number and distribution, as well as morphology and chemical properties of specific neuron subclasses in histologically prepared human cortical tissue of schizophrenic subjects in the region that synaptic alteration was suggested by in-vivo functional and structural imaging (SPECT) and psychological testing. This will provide psychological, functional and imaging parameters which could be related to circuitry organization in adult and developing subjects. These parameters might serve as a normative for diagnosis of disorders characterized with impairment of higher cognitive functions.
WP4 incorporates the analysis of association of pharmacogenetic markers and treatment response.
RESULTS
WPA XVII World congress of psychiary, Berlin 2017, Bosnjak D, et al.
WPA XVII World congress of psychiary, Berlin 2017, Makaric P, et al.